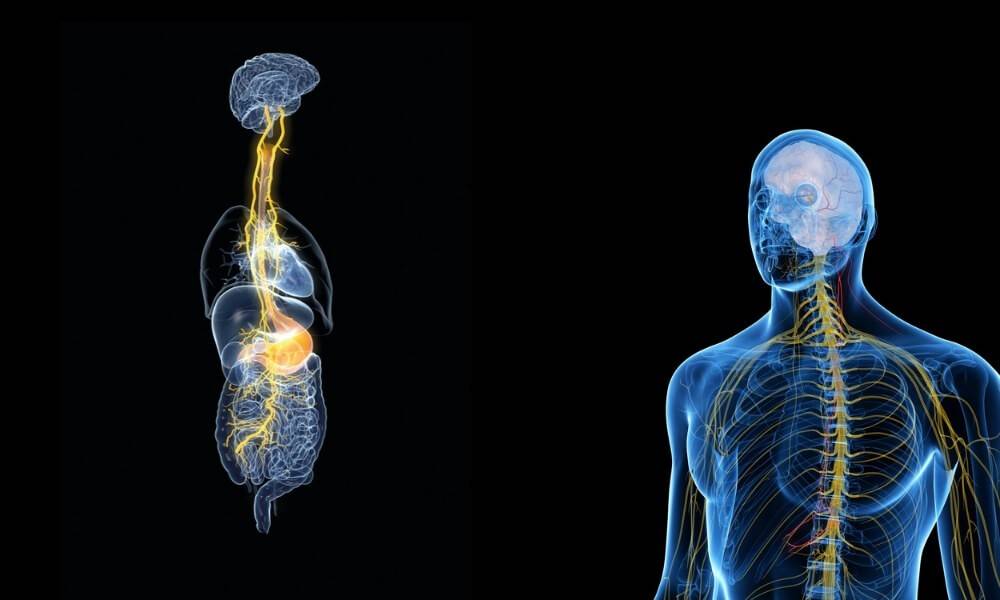
The vagus nerve is one of 12 cranial nerves in the body that link various parts to the brain. The vagus nerve — also called cranial nerve X (as in Roman numeral) — is the longest nerve, and runs from the brain stem to the colon in two parallel routes.
What Does the Vagus Nerve Do?
The vagus nerve provides sensory and motor functions to the organs and surrounding skin, from the lower brain stem to the upper colon.
- The sensory functions include sensations felt on and in skin and muscle, and in the organs.
- The motor functions stimulate muscles and contractions in various body parts, including the heart and digestive system.
“Vagus” is the Latin word for wandering, which is a good way to think about the vagus nerve. It’s a vagabond nerve, wandering up and down the torso to gather information to use, to direct actions and reactions.
The gag reflex is one way doctors test the vagus nerve to make sure it’s working properly. When your doctor looks inside your mouth, tells you to stick out your tongue and say “ah,” and touches something (usually a cotton swab) against the back of your throat, you gag. Gagging indicates major vagus nerve functions are OK. Not gagging, though, indicates a problem.
Vagus Nerve Disorders Include Gastroparesis
The vagus nerve covers a lot of ground, so vagus nerve damage tends to be local, unlike a typical virus that can cause a headache with an upset stomach. Ongoing digestive problems may be caused by gastroparesis, a condition that interferes with the contractions that help the stomach empty its contents.
A patient with gastroparesis may vomit undigested food hours after eating. Or he may suddenly feel full or lose his appetite after eating a small amount. There may be abdominal pain, or bloating since the stomach isn’t emptying properly, and weight loss.
Some patients experience acid reflux, which is when stomach acids back up into the esophagus. (This can also cause hoarseness, another symptom of possible vagus nerve damage.) Because eating and digestion are affected, patients may also have problems with blood sugar fluctuations.
Gastroparesis can be related to diabetes, particularly in patients who have a difficult time controlling their blood sugar levels. It also occurs after a patient has part of the vagus nerve removed in the stomach or other gastrointestinal surgery. However, about one-third of gastroparesis diagnoses have no definitive cause.

Stress May Cause Vagus Nerve Damage
The vagus nerve is, after all, a nerve, so it’s no surprise that vagus nerve damage can come from certain triggers.
Do you feel queasy or even faint at the sight of blood? This may be a sign of the vagus nerve overreacting to stimuli, in this case, visual and, perhaps, sensory. The vagus nerve tells the heart to slow down; if this happens too quickly, your muscles lose control and you faint. This condition, called vasovagal syncope, is pretty common.
Other vagus nerve triggers include standing for too long, exposure to extreme heat, or overwhelming fear.
Vagus Nerve Damage Treatment
Treating a damaged vagus nerve means relieving symptoms and avoiding environments that seem to trigger nerve overstimulation. Behavioral changes can help a lot:
- Avoid going outdoors in extremely hot weather and drink plenty of water (even when you’re indoors).
- Look away when you have blood drawn, and don’t volunteer as a first responder.
- Dietary changes can help with gastroparesis, particularly for people with diabetes.
Antinausea medication can ease the worst gastroparesis symptoms, and there are a few medications that stimulate stomach contractions.
Moderate, regular exercise also seems to relieve an overstimulated vagus nerve. Also, a chiropractor can ease the condition. If you have questions about unexplained pain or discomfort, contact us as soon as possible!